Cardiovascular disease (CVD) is the leading cause of death globally, taking an estimated 17.9 million lives each year. Over a 30-year period, deaths from CVD have jumped across the world — from 12.1 million in 1990 to 20.5 million in 2021 — according to a new report from the World Heart Federation (WHF), shedding light on an underlying crisis that has long remained unaddressed.
While cholesterol has conventionally shouldered the blame for heart disease, this singular focus has overshadowed other critical factors contributing to the escalating number of fatalities. Blaming heart disease solely on cholesterol oversimplifies the problem and diverts attention from the array of factors contributing to the public health crisis.
Functional medicine practitioners have been at the forefront of this dialogue worldwide. Senior practitioners deplore that the lack of emphasis on personalised medicine, the foundation of epigenetics, is why nearly 50 per cent of all heart attacks and strokes occur in patients with ‘normal’ cholesterol levels. It means that in at least half of these cases, healthcare providers may not have addressed the underlying risk factors that led to the heart attack.
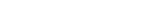
Functional medicine expands on the unique impacts of cholesterol, lipoproteins, insulin dysfunction, inflammation, and oxidative stress, which enables practitioners like me to now provide my patients the added security of knowing how their decisions (lifestyle and/or pharmaceutical) are impacting their global cardiometabolic risk score. While they seem to be different types of conditions, cardiovascular and metabolic dysfunctions share similar causes, including inflammation, insulin resistance and stress.
THE STATIN DEBATE
The ubiquity of statin drugs worldwide is disturbing. Statins have become a doctor’s first line of defence; the best resort, not the last resort. And this is despite the fact that these drugs while being touted as a grand cure-all have done nothing to stop the rise of heart disease worldwide. CVD is still the number-one killer; in fact, it has become a worldwide epidemic.
Since cholesterol can be lowered with statin drugs, pharmaceutical companies have been very effective in ‘educating’ doctors to look only at LDL and total cholesterol as the primary cardiovascular risk markers. Statins primarily target cholesterol levels, providing a false sense of security that the underlying issues are being resolved. Why aren’t physicians thinking beyond prescriptions and questioning an approach that clearly isn’t working?
The use of statins doesn’t come free, they have a cost or risk associated with them (see box Risks Associated With Statin Use). Statins work by inhibiting an enzyme called HMGCoA Reductase, which is involved in the production of cholesterol in the liver. However, this enzyme is also involved in the synthesis of CoQ10, which is involved in the process of energy production in every cell. So statin use can result in muscle pains, body pains, low energy levels and a host of other issues.
The Statin Effects Study has been published in journals such as the Journal of the American Heart Association, the Archives of Internal Medicine, Controlled Clinical Trials, and Annals of Internal Medicine.
THE DARK SIDE OF HAVING LOW CHOLESTEROL
Most importantly, have we ever stopped to think about the ramifications of having very low cholesterol levels? It is arguably more dangerous than having high cholesterol. Cholesterol plays an important role in organ and tissue repair, it helps produce stem cells. If cholesterol is too low, blood vessels become stiffer and are more likely to break. There is an increased risk of death.
Some significant side effects of low cholesterol are:
ISCHEMIC STROKE: Total cholesterol below 160mg/dl was associated with higher ischemic stroke mortality in a study Low Serum Cholesterol Level and Increased Ischemic Stroke Mortality by Hisako Tsuji, MD, in the Journal of the American Medical Association. Tsuji had tracked 16,000 participants over a 10-year period for this study.
INTRACRANIAL HEMORRHAGE (ICH): In a 2012 study (Low cholesterol as a risk factor for primary intracerebral hemorrhage: A case-control study by Valappil A.V., Chaudhary N.V., Praveenkumar R., Gopalakrishnan B. and Girija A.S.), serum cholesterol below 160mg/dl increased the odds for ICH 2.25-fold.
MOOD CHANGES: Low serum cholesterol has been associated with an increase in violent or impulsive behaviour, depressed mood, and suicidality, especially among males. In one study (The Relationships between Cholesterol and Suicides: An update in ISRN Psychiatry by De Beradis D., Marini S., Piersanti M.,et al) the risk of suicide attempts increased 7.33-fold in men and 15.6-fold in women in the lowest cholesterol quartile compared to subjects in thehighest quartile.
FORGOTTEN AND IGNORED: TRIGLYCERIDES AND HDL
Relying on total cholesterol alone is bad medicine. It’s 1960s thinking, and science has evolved dramatically since then. When it comes to heart health, LDL and total cholesterol numbers are overrated, while triglycerides, HDL and LDL particle numbers are underrated.
There are two major classifications of LDL cholesterol particles that can be measured. Pattern A is the large fluffy and generally harmless kind. Pattern B is the small, dense, potentially dangerous kind that is described as “bad”. Pattern B can easily penetrate the arterial wall, compromising your heart health. This is what we want to avoid at all costs. So, knowing the breakdown of cholesterol is critical in determining overall heart health. NMR lipid Profile is the test for measuring your LDL particle number and size.
So having small LDL particles is bad, since that leads to atherosclerosis, and these small dense LDL particles greatly increase when triglycerides are simultaneously high and HDL cholesterol is low.
The biggest marker of poor cholesterol health is elevated blood levels of triglycerides, which is one of the most important markers for determining your overall metabolic health. There is a strong inverse relationship between triglycerides and HDL cholesterol. One very simple way to elevate triglycerides is simply eating carbohydrates. Consuming fewer carbs and more healthy saturated fats bring the HDL levels up quite nicely, and so does regular exercise.
The ratio of triglycerides-toHDL goes hand in hand with determining whether or not you have a prevalence of small LDL particles. Conversely, when the ratio is low, there aren’t many small LDL particles, meaning you are at a reduced risk of heart disease. So, if you don’t have access to measuring your small LDL-P, the next best markers to look at are your triglycerides and HDL. Aiming for triglycerides lower than 70, and HDL 60 and above is ideal.
INSULIN RESISTANCE Insulin resistance and the resulting hyperinsulinemia can promote inflammation, oxidative stress, endothelial dysfunction and abnormal lipid metabolism, all of which contribute to the development of cardiometabolic diseases. Functional medicine approaches these issues by addressing the underlying root causes and imbalances that contribute to insulin resistance and cardiovascular risk, rather than just treating symptoms. These include a person’s diet, level of physical activity, stress level, sleep quality, environmental exposures, gut health and genetic predispositions.
ASSESSMENT OF CARDIOMETABOLIC RISK
According to the International Diabetes Federation, the following criteria describes a diagnosis of cardiometabolic syndrome:
1: Central Obesity, or increased waist circumference
2: Elevated triglycerides >150mg/dl (drug treatment for hypertriglyceridemia is an alternate indicator)
3: Low HDL-C: Less than 40mg/ dl in males and 50mg/dl in females
4: Elevated blood pressure: Systolic BP of 130mmHg or more and/or diastolic BP higher than 85mmHg (or antihypertensive drug treatment in)
5: Elevated fasting glucose: Elevated or more than 100mg/dl (drug treatment of elevated glucose is an alternate indicator) Additional clinical indicators that help in the assessment are obesity, acrochordon (skin tags), acanthosis nigricans, decrease in pinprick, temperature, vibration and pressure sensation (using a 10g monofilament pressure sensation at the distal halluces), ulceration, and Tinea pedis.
INFLUENCING FACTORS
A variety of factors including celiac disease, polycystic ovary syndrome (PCOS), gestational diabetes and stress can increase the likelihood of metabolic syndrome.
CARDIOMETABOLIC CONDITIONS AND THE MICROBIOME
The gut microbiome plays a crucial role in cardiometabolic health. Studies have shown that certain families of gut bacteria can influence cardiovascular health, BMI, and lipid levels. The microbiome can generate metabolites that impact host physiology and metabolic inflammation, including the production of trimethylamine N-oxide (TMAO), associated with coronary artery disease and stroke. Gut microbial composition has been linked to arterial stiffness and insulin resistance.
DIETARY IMPACTS
This research is exciting in part because the microbiome changes rapidly in response to diet, making nutrition an important part of the microbiome-cardiometabolic equation. For example, research suggests that diets naturally rich in polyphenols and/or long-chain n-3 polyunsaturated fatty acids found in fatty fish, flaxseeds, walnuts, chia seeds, etc., may significantly increase gut microbial diversity and bifidobacterial concentrations impacting glucose and lipid metabolism.
Also, bioactive compounds found in Mediterranean-style diets potentially adjust the ratio of Firmicutes/ Bacteroidetes in the microbiome, improving the management and prevention of metabolic syndrome. Treating the gut using diet, probiotics, prebiotic foods, and other therapies may reduce risks for many cardiometabolic patients.
Here, in this Part-I of this article, we have uncovered a broader and more comprehensive approach to the assessment of cardiovascular risk factors that go beyond lipids alone. We have discovered how addressing metabolic syndrome is of paramount importance. It highlights the multifaceted nature of cardiovascular risk assessment. In Part-II, we will shift gears from assessment to treatment and delve into the realm of diet and lifestyle modifications that can effectively reverse or prevent cardiometabolic conditions. Stay tuned for a journey towards a healthier heart!