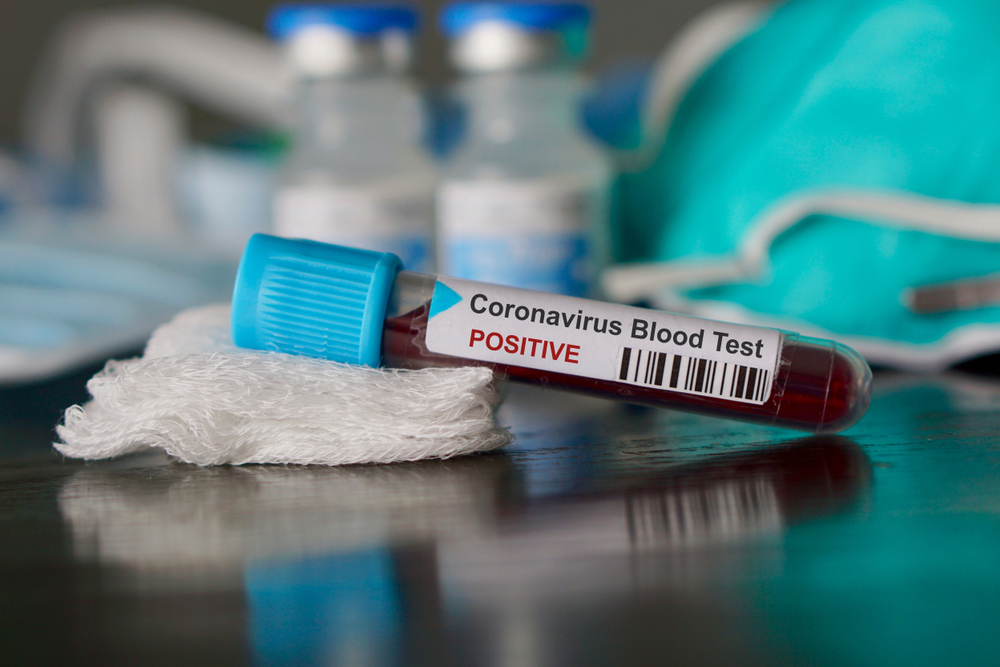
The Union health ministry has often claimed credit for the country’s early countermeasures against the coronavirus but has held back key quantitative data that health experts say could provide insights into the nation’s state of preparedness and outbreak patterns.
Medical experts tracking the country’s response to its rising coronavirus counts said high-granularity quantitative data showing how and where the outbreak is spreading and hospital inventories of critical care beds and ventilators — in states and districts — would help guide evidence-based decision making.
The Centre updates its national and state numbers of coronavirus patients, cured patients and deaths on its website, providing significant information about nationwide and state-wise trends of the outbreak.
But experts say it is not easy to access high-resolution data.
The health ministry, for instance, has not officially listed coronavirus hotspots in the country. On Thursday, the ministry uploaded on its website a document that said: “Although there is no evidence for widespread community transmission, 20 existing and 22 potential hotspots have been identified.”
But a senior health ministry official, deputed to brief the media on Thursday afternoon hours after the ministry had uploaded the document and asked about the hotspots, said the numbers keep changing.
“In our understanding, wherever there is a case, that area becomes a hotspot for us, and we adopt containment measures under our protocols,” said Lav Agarwal, joint secretary in the ministry. “If the number of cases grows in an area, to that extent, we increase our interventions there.”
“As our cases increase, the number of our hotspots changes,” he said.
Infectious disease and public health specialists familiar with the containment and response strategy view Agarwal’s response as an attempt to hold back naming hotspots that could ironically hamper the country’s response to the outbreak.
“Maybe they want to avoid panic among the public, but making such information available will facilitate a coordinated, calibrated response,” said Oommen John, a public health expert at The George Institute of Global Health, New Delhi.
“Several corporates and private healthcare institutions are offering to help the government. Greater transparency is always better in such circumstances,” he said.
The Association of Healthcare Providers of India, a body of private hospitals, had asked for a list of hotspots so it could prepare its member hospitals where needed. “The faster we know, the earlier we can identify hospitals,” said AHPI executive director Girdhar Gyani.
Gyani said some states have contacted AHPI members and requested hospitals. Rajasthan, for instance, has told the AHPI members that they would need to be ready to serve at a “two-hour notice”, he said.
The health ministry did not respond to a query sent by The Telegraph about concerns among experts about such information gaps. But a senior health official asserted that the health ministry and other arms of the government — at the Centre and state level — are doing their best to respond to an “unprecedented situation”.
Agarwal himself has often asserted that the government has responded in a graded and escalating manner as the situation has demanded.
Union health secretary Preeti Sudan first wrote to states asking them to enhance their preparedness and hospital infrastructure in January and followed it up with multiple requests. But the outcomes of those requests measured through critical-care beds or ventilators remain unclear.
During its briefings, the health ministry has periodically revealed information about new equipment ordered. For instance, it said last week, the government had ordered 1,800 ventilators. On Wednesday, the health ministry said the railways had offered to create 320,000 quarantine beds, including 80,000 isolation beds on train coaches.
Agarwal said on Thursday that the government had ordered 15 million units of personal protective equipment and 10 million N95 masks.
But critical-care specialists point out that without baseline numbers, the values of any incremental additions remain unclear.
“District-level distribution of critical care beds and ventilators would help — hopefully, the health ministry has this information. But it would help if this is made public,” said a scientist involved in mathematical modelling of the outbreak.
“If the rise in the numbers continues, such information would allow policy makers to quickly map counts with areas where beds or ventilators are likely to be in short supply and take steps to channel resources there.”
The health ministry has thus far not revealed the numbers of healthcare workers in India who might have contracted the infection. Unverified social media posts suggest that in Delhi alone eight doctors have tested positive. Social media posts suggest the number across India could be around 50.
“When a healthcare worker gets infected, there could be a problem — either with availability of the personal protective equipment or perhaps in training and use of such equipment,” said Anant Bhan, a physician and bioethics expert. “It is important to know where such infections have occurred so that they can be addressed.”
WHY WE ASK
How the information can help the response
Question: What are the numbers and the locations of ‘hotspots’ in the country?
Why? The identity of the hotspots will allow healthcare staff and private healthcare institutions to respond better to the requirements there and prompt public to remain even more vigilant.
Question: How many critical care beds/ventilators do the government and private hospitals have at the state and district level? Which specific states, areas, or hospitals are currently experiencing shortages of masks, gloves or other personal protective equipment?
Why? The government’s own supply chain, policy-makers and epidemiology researchers trying to model the future course of the epidemic could use this information to map better specific areas in need with the available resources.
Question: In which institutions have healthcare workers been infected in the country? How many?
Why? A healthcare worker getting infected might be an indicator that the hospital may be experiencing a shortage of personal protective equipment or staff has received inadequate training. Both possibilities require corrective action.